MSI GS63VR 6RF i7 2.6GHz 8GB SSD256GB HDD1TB GTX1060 Win10 15.6型 ノート
(税込) 送料込み
商品の説明
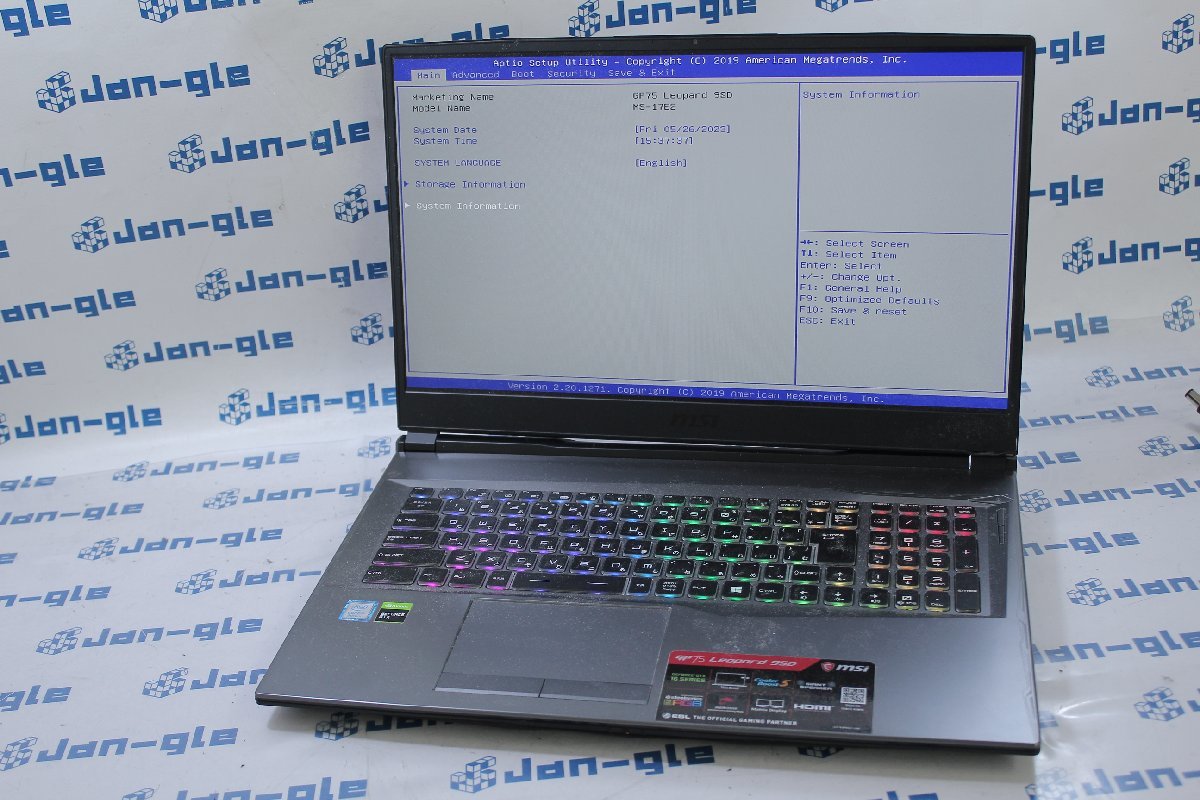
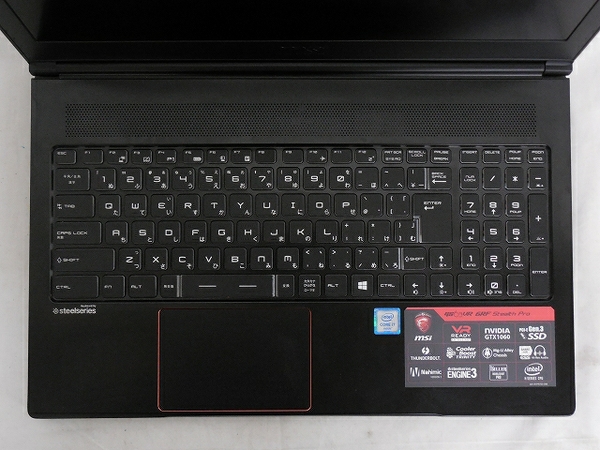
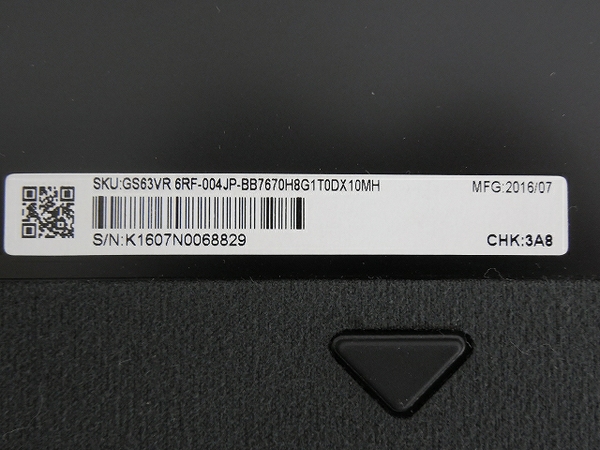
メーカー名MSI型番 GS63VR 6RFシリアル K1607N0068829メーカー保証 無リカバリ領域 有OS Wndows 10 Home 64bitCPU Intel Core i7-6700HQ 2.60GHzメモリ 8GBストレージ SSD256GBHDD1TBグラフィック NVIDIA GeForce GTX 1060Intel HD Graphics 530ディスプレイ 15.6型オフィスソフト 無カラー ブラック系動作 通電、キーボード、トラックパッド、USBポート、Wi-Fi、サウンド、カメラ付属品 電源コード、ACアダプタ、マニュアル類、元箱61029円MSI GS63VR 6RF i7 2.6GHz 8GB SSD256GB HDD1TB GTX1060 Win10 15.6型 ノートその他MSI GS63VR 6RF i7 2.6GHz 8GB SSD256GB HDD1TB GTX1060 Win10 15.6型 ノート Ltd. GS63VR 6RF(ノートパソコン)のMicro-Star International Co., Ltd. GS63VR 6RF(ノートパソコン)の
MSI GS63VR 6RF-004JP 価格比較 - 価格.com
Micro-Star International Co., Ltd. GS63VR 6RF(ノートパソコン)の
Micro-Star International Co., Ltd. GS63VR 6RF(ノートパソコン)の
Micro-Star International Co., Ltd. GS63VR 6RF(ノートパソコン)の
Micro-Star International Co., Ltd. GS63VR 6RF(ノートパソコン)の
2023年最新】Yahoo!オークション -msi gsの中古品・新品・未使用品一覧
2023年最新】ヤフオク! -msi gs(コンピュータ)の中古品・新品・未使用
2023年最新】Yahoo!オークション -msi(ノートブック、ノートパソコン
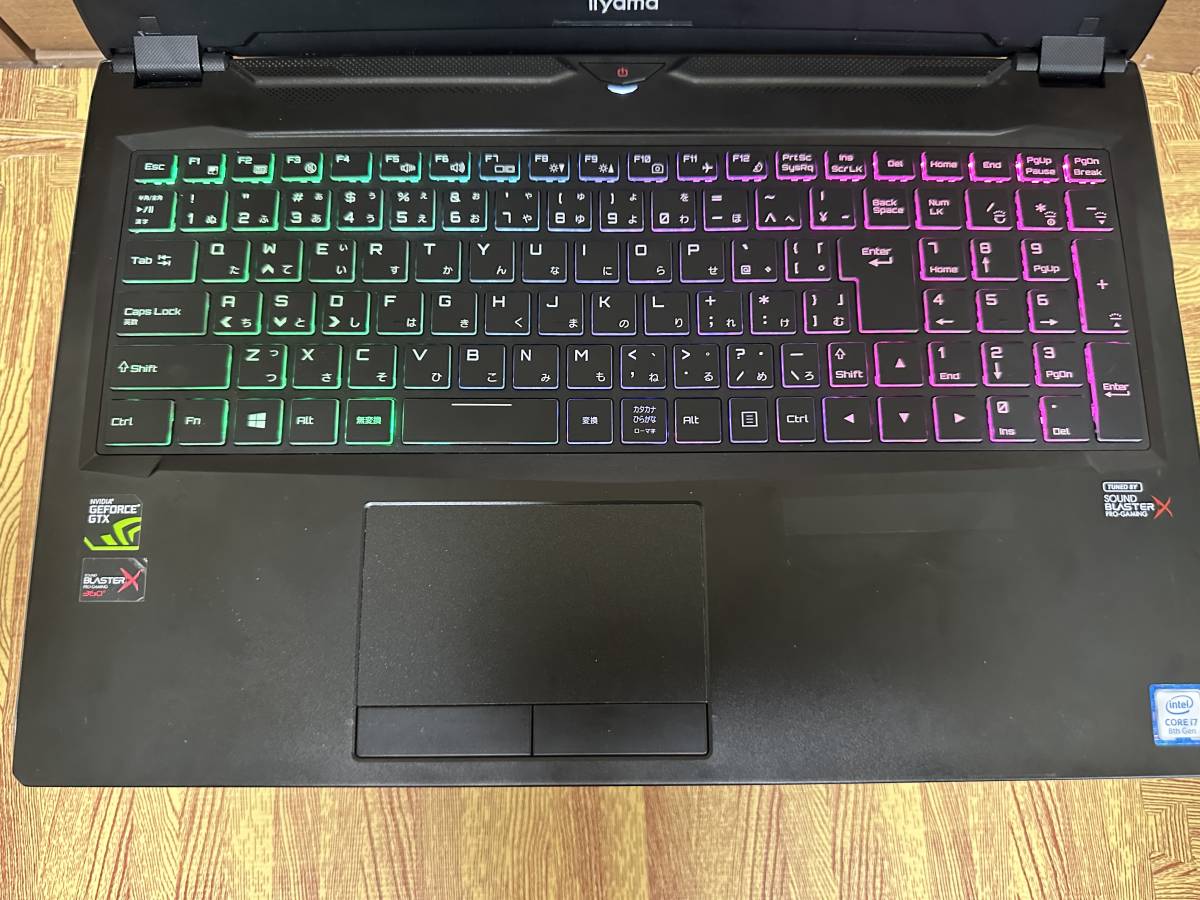
◇iiyama☆ゲーミングノートPC P95xER Intel Core i7-8750H 2.20GHz
◇iiyama☆ゲーミングノートPC P95xER Intel Core i7-8750H 2.20GHz
2023年最新】Yahoo!オークション -msi(ノートブック、ノートパソコン
2023年最新】ヤフオク! -msi ノートパソコン(Windows)の中古品・新品
2023年最新】ヤフオク! -msi ノートパソコン(Windows)の中古品・新品
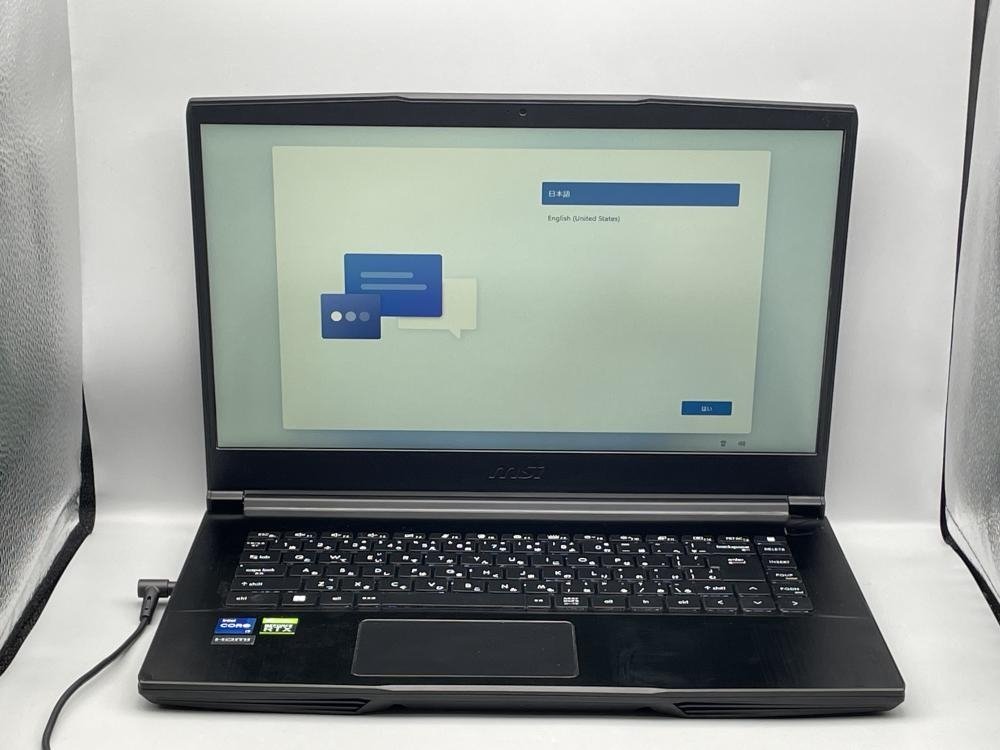
MSI ゲーミングノートパソコン GS63VR 6RF-004 ジャンク-
◇iiyama☆ゲーミングノートPC P95xER Intel Core i7-8750H 2.20GHz
2023年最新】ヤフオク! -msi ノートパソコン(Windows)の中古品・新品
2023年最新】Yahoo!オークション -msi(ノートブック、ノートパソコン
2023年最新】ヤフオク! -msi ノートパソコン(Windows)の中古品・新品
2023年最新】ヤフオク! -msi gs(コンピュータ)の中古品・新品・未使用
2023年最新】ヤフオク! -msi ノートパソコン(Windows)の中古品・新品
2023年最新】Yahoo!オークション -msi(ノートブック、ノートパソコン
◇iiyama☆ゲーミングノートPC P95xER Intel Core i7-8750H 2.20GHz
2023年最新】Yahoo!オークション -ゲーミング ノート(ノートブック
◇iiyama☆ゲーミングノートPC P95xER Intel Core i7-8750H 2.20GHz
◇iiyama☆ゲーミングノートPC P95xER Intel Core i7-8750H 2.20GHz
2023年最新】ヤフオク! -msi ノートパソコン(Windows)の中古品・新品
2023年最新】Yahoo!オークション -msi(ノートブック、ノートパソコン
☆ハイスペック&コンパクトGALLERIA GCR1660TGF-QC-G/Core i7-9750H
ヤフオク! -「geforce2」(その他) (ノートブック、ノートパソコン)の
2023年最新】Yahoo!オークション -ゲーミング ノート(ノートブック
☆ハイスペック&コンパクトGALLERIA GCR1660TGF-QC-G/Core i7-9750H
2023年最新】ヤフオク! -msi ノートパソコン(Windows)の中古品・新品
2023年最新】Yahoo!オークション -ゲーミング ノート(ノートブック
2023年最新】Yahoo!オークション -msi(ノートブック、ノートパソコン
2023年最新】Yahoo!オークション -msi(ノートブック、ノートパソコン
ヤフオク! -「geforce2」(その他) (ノートブック、ノートパソコン)の
2023年最新】Yahoo!オークション -ゲーミング ノート(ノートブック
☆ハイスペック&コンパクトGALLERIA GCR1660TGF-QC-G/Core i7-9750H
MSI ゲーミングノートパソコン GS63VR 6RF-004 ジャンク-
商品の情報
メルカリ安心への取り組み
お金は事務局に支払われ、評価後に振り込まれます
出品者
スピード発送
この出品者は平均24時間以内に発送しています